Introduction
The existence of BCR-ABL+ AML as an entity distinct from BC-CML is controversial. The WHO recently recognized BCR-ABL+ AML, but with the caveat that it is poorly characterized (Khoury, 2022). Clinically, BCR-ABL+ AML is associated with high risk of relapse (Neuendorff, 2018). Further, acquired BCR-ABL mutations have been identified as a cause of relapse on FLT3 inhibitors (McMahon, 2019). We hypothesize that BCR-ABL+ AML can be distinguished as a distinct biologic entity from BC-CML by the observation of BCR-ABL as a sub-clonal rather than a founder mutation in leukemogenesis.
Methods
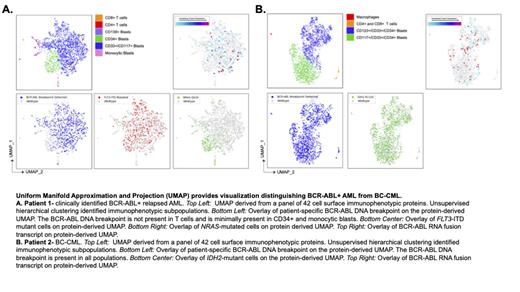
To test the utility of multi-omic single cell (SC) sequencing in determining tumor phylogeny and identification of BCR-ABL+ AML vs BC-CML, we analyzed bone marrow samples from 4 patients (pts): 1 relapsed AML with clinical development of a new BCR-ABL fusion at the time of relapse, and 3 newly diagnosed BC-CML (2 myeloid, 1 lymphoid). We performed high-throughput SC DNA sequencing with simultaneous cell-surface immunophenotyping and targeted RNA sequencing for BCR-ABL fusion proteins (Mission Bio Tapestri). All SC DNA sequencing included pt-specific primers for BCR-ABL DNA breakpoints, which were previously identified using nanopore-based technology for sequencing long strands of DNA.
Results
We analyzed 19,197 single cells (median 1995 cells/pt). Multi-omic SC technology differentiated BCR-ABL+ AML from BC-CML by confirming the fusion arose as a branch mutation from a founding leukemic clone and was not present in all leukemic populations.
In Patient 1, who was sampled at time of AML relapse, we identified pathogenic FLT3 ITD and NRAS Q61K mutations. FLT3 co-mutated with either the BCR-ABL DNA breakpoint or NRAS in the same single cell and clone, while the BCR-ABL DNA breakpoint and NRAS were not co-mutated. Phylogenetic reconstruction determined FLT3 to be a founding mutation, which later branched into FLT3/BCR-ABL and FLT3/ NRAS co-mutant subclones. Further, the FLT3-ITD/BCR-ABL and FLT3-ITD/ NRAS subclones had distinct immunophenotypes. Blasts harboring the BCR-ABL DNA breakpoint were predominantly identified in the CD117+/CD33+ population (60.2% of cells) compared to CD34+ (16.4% of cells, p <0.001) and blasts with monocytic differentiation (19.1% of cells, p = 0.02). Notably, BCR-ABL+ cells were not identified in T cells. NRAS mutations were predominantly identified in both CD34+ and monocytic blasts. Together, these data support BCR-ABL arising late within the evolutionary history of this pt's AML.
By contrast, in Patients 2 and 3 with myeloid BC-CML, the BCR-ABL DNA breakpoint and corresponding BCR-ABL fusion were detectable in all cell populations, including blasts as well as immunophenotypically normal T cells, B cells, and macrophages. In Patient 2, we identified an IDH2 R132C mutation co-mutated with BCR-ABL. Phylogenetic reconstruction determined the IDH2 mutation arose as a branch from a founding BCR-ABL+clone. Unlike the BCR-ABL breakpoint, which was present in all cell populations, the IDH2 mutation was only identified in immunophenotypically-defined CD33+/CD34+/CD117+ myeloid blasts and was absent from bystander T cells and macrophages.
Finally, Patient 4had a clinical diagnosis of lymphoid BC-CML. Like Patients 2 and 3, the BCR-ABL DNA breakpoint and corresponding RNA fusion were present in all immunophenotypically-defined blast populations. Unlike Patients 2 and 3, however, BCR-ABL was absent from immunophenotypically normal CD4+ and CD8+ T cells, macrophages, and monocytes. Additional pts are needed to determine whether this pattern is consistent with all lymphoid BC-CML or whether this pt's biology may have been closer to BCR-ABL+ acute lymphoblastic leukemia (ALL).
Conclusions
Multi-omic SC technology can distinguish BCR-ABL+ AML from myeloid BC-CML and provide direct confirmation that lineage-restriction of BCR-ABL potentially clarifies the diagnosis of discrete Ph+ leukemias. Future studies are needed to understand the role of RT-PCR based BCR-ABL1 testing as a marker of minimal residual disease in pts with BCR-ABL+ subclones, the impact of BCR-ABL as a potential driver of AML resistance, and the utility of BCR-ABL inhibitors in leukemias with late-arising BCR-ABL+ clones.
Support: U10CA180821, U10CA180882, U24CA196171; https://acknowledgments.alliancefound.org. Clinicaltrials.gov Identifiers: NCT00048958, NCT00899223, NCT00900224
Disclosures
Kennedy:Astellas: Consultancy. Dhingra:Mission Bio Inc: Current Employment. Gulati:Mission Bio Inc: Current Employment. Sciambi:Mission Bio Inc: Current Employment. Logan:Amgen, Autolus Therapeutics, Kadmon, Kite, Pharmacyclics, Talaris: Research Funding; AbbVie, Amgen, Actinium, BMS, Pfizer, Sanofi, Takeda: Consultancy. Perl:Astellas: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Abbvie: Consultancy, Honoraria, Research Funding; Daiichi-Sankyo: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bayer: Research Funding; FujiFilm: Research Funding; Syndax: Research Funding; Forma: Consultancy; Foghorn: Consultancy; Beat AML: Other: Participation on a Data Safety Monitoring Board or Advisory Board; BerGen Bio: Honoraria; Genentech: Honoraria; Immunogen: Honoraria; BMS: Honoraria; Aptose: Honoraria; Rigel: Honoraria; Actinium: Honoraria. Stock:Kite: Consultancy; Kura: Research Funding; Servier: Other: Data Safety Monitoring Board/Advisory Board; Newave: Honoraria; Amgen: Honoraria; Jazz Pharmaceuticals: Consultancy, Honoraria; Glaxo Smith Kline: Consultancy. Uy:Jazz: Other: Advisory Board. Eisfeld:Karyopharm Therapeutics: Other: spouse employment; Astra Zeneca: Honoraria, Other: CEI Advisory Board; OncLive: Honoraria. Smith:ERASCA: Research Funding; Genentech: Honoraria; Abbvie: Honoraria, Research Funding; Cellgene: Other: Clinical trial funding; Zentalis: Other: Clinical trial funding; Revolution Medicines: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal